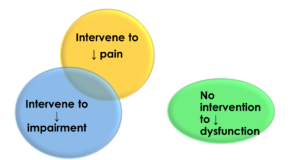
Choices of interventions for musculoskeletal pain syndromes: decrease pain, improve impairment, resolve dysfunction
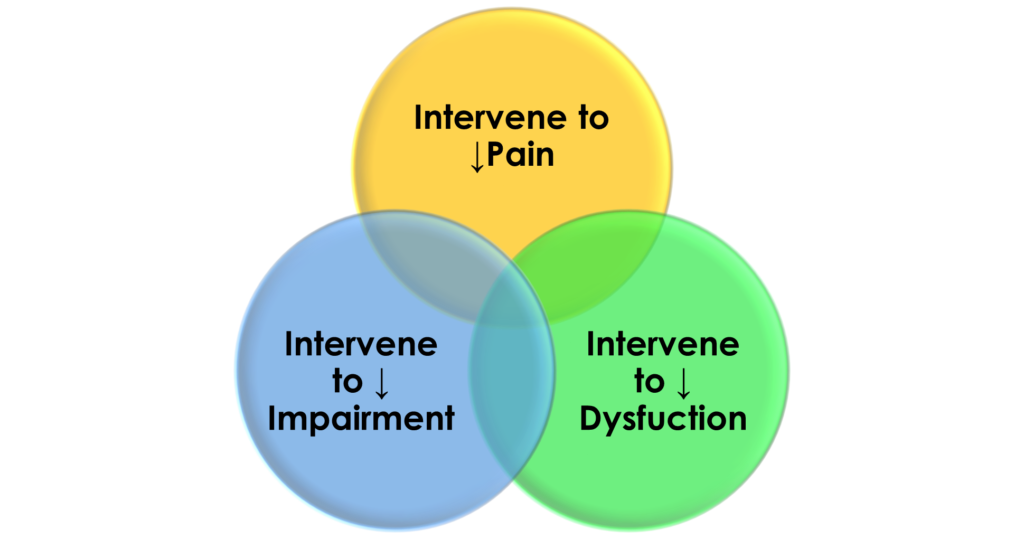
There are multiple and varied interventions that can tackle the contributing factors of pain, impairment, and dysfunction that occurs with musculoskeletal pain syndromes.
Pain impairs an individual's ability to function
Impairment is loss of use or derangement of any body part, organ system, or organ function.
Dysfunction is an alteration of an individual’s capacity to meet personal, social, or occupational demands because of an impairment.
In a treatment or intervention-based classification, the clinician and patient make decisions based on the aim, focus, or rationale.
Examples of interventions which the aim is:
- Alleviating pain are analgesic pain medication, topical analgesic medications, acupuncture, dry needling, and electrical stimulations. The assumption is if the pain is relieved the dysfunction will be resolved.
- Improving impairment is surgery, joint replacement surgery, strengthening exercises, and flexibility exercises. The assumption is if the impairment is addressed the dysfunction will be resolved
- Resolving dysfunction are movement pattern training, motor skill training, functional training, gait training, motor learning, and coaching. The assumption is if the dysfunction is resolved the pain will be resolved.
- Overlappings are isometric strengthening exercises and aerobic exercises which have been shown to improve the impairment of weakness and reduce pain. Elanna Arhos and colleagues have shown specific functional movement training of individuals with patella femoral pain improves impaired hip muscle strength without using traditional strengthening exercises.
My observation is the most prevalent approach towards musculoskeletal pain syndromes is to provide interventions aimed at decreasing pain and decreasing impairment without using interventions that aim towards decreasing dysfunction.
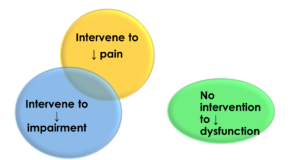
An outcome of choosing interventions to alleviate pain and impairment without using interventions that address the dysfunction is returning to the previous functional activities moving in the same style/manner as prior to injury which may be deviant and less than optimal.
Irene Davies et. al in 2016 reviewed literature related to running injury and suggests strengthening exercise alone is not enough to alter running mechanics.
Inga Kraus and colleagues in 2020 showed a 12-week exercise program of strengthening and flexibility exercises in patients with hip osteoarthritis had no influence on gait deviations.
Jennifer Brach et.al in 2013 when dealing with older individuals with an increased risk of falling suggest if walking is the problem, then intervention should primarily focus on the task of walking through motor skill-based training and not impairment-based exercise intervention alone.
Jacqueline Bahr and colleagues 2021 show despite alleviating the pain and impairment of osteoarthritic hip or knee joint by surgically replacing the joint the gait dysfunctions continue.
What does an intervention aimed at alleviating dysfunction look like?
Movement pattern training or motor skill training is a novel approach that directly addresses the performance of painful and limited functional activities that the client chooses to address through challenging practice to improve performance and decrease pain. It involves supervised massed practice of challenging functional activities that are difficult to perform because of pain. Emphasis is on changing the deviant movements and alignments relevant to the person’s specific movement system impairment syndromes.
An example is when ascending and descending stairs provide curing, prompting, and feedback to maintain a level pelvis, no side bending of the trunk, and keep the knee over the second toe. In contrast, strength and flexibility exercises aim on improving the strength of muscles and improving flexibility of the hip muscles. In the above example strengthening exercises would involve side-lying leg lifts, clamshell exercises, and lateral steps with elastic bands.
Is movement pattern training effective and efficient?
Movement pattern training has been successfully applied to musculoskeletal pain syndromes of the low back, shoulder, hip/groin, and knee.
Linda van Dillon and colleagues in a well-designed study of individuals with chronic low back pain who received movement pattern training had greater short-term and long-term (12 months follow-up) improvements in function compared to those who received strengthening and flexibility exercises.
This approach can be applied to other musculoskeletal pain syndromes where strategies of movements and postures used across the day are associated with a person’s pain and functional limitations.
A case example using movement pattern training for hamstring tendinopathy
A veteran marathon runner reporting recurring left hamstring and Achilles tendinopathy interfering with training limiting her weekly long-distance runs. After 2 to 3 miles of running right, calf muscle pain resulted in limping.
Previous interventions aimed at relieving pain and impairment, including stretching exercises, strengthening exercises, cold packs, dry needling, foam rolling, massage, and shoe therapy were ineffective.
Two-dimensional slow-motion video analysis of running revealed asymmetrical movement running of excessive rotation of the trunk to the right, and the right foot crossing the mid-line of the body. Rather than add, alter, or escalate previous inventions aim at pain and impairment, intervention whose aim is to alter functional movement running is appropriate.
Cueing, prompting, and feedback consistent with her preferred learning sense to push harder with the uninvolved right foot, emphasize the movement of the right arm across the body to increase the rotation of the trunk to the left is to the point. The motor pattern gait training altered deviant performance within one treatment session. After having repeated practice over several days, she can return to 20-mile training runs symptom-free.
Ideally, a comprehensive approach to the management of musculoskeletal pain syndromes is to use interventions that aim to alter all three parameters pain, impairment, and dysfunction.
However often, interventions aim to resolve just pain and impairment without consideration for interventions aimed at resolving the dysfunction.
Why is that?
There are likely many potential reasons. One reason is traditional healthcare for musculoskeletal pain syndromes is provided in setting not conducive to observing and intervening in functional movements. Exam rooms in the clinical setting do not allow observing a tennis serve, picking up grandchildren, or standing long enough to prepare a meal without back pain. Another is when the clinician asks the patient what can I help you with? The patient responds, “I have shoulder pain.” The focus then becomes the pain rather than the patient saying, “I have difficulty wiping my butt because my shoulder hurts.” Here the focus becomes being able to whip the butt without pain rather than focusing on the pain. Another is it can be more challenging and requires the more active involvement of the patient to coach and learn to move in a more optimal manner than it is to passively lie on a table and receive a massage.
If you are a patient, consider the following:
Be sure to share with your healthcare clinician your expectations and desires regarding those activities or functions that you are having difficulty doing because of the pain.
Ask if is there more I can be doing besides the pain-relieving treatments, and remedial exercises to return to my favorite activity/sport.
Ask what I can do in the future to prevent this problem from recurring.
If you are a healthcare practitioner, consider the following:
Choose interventions that directly address the results of the patient self-report specific functional score.
When possible, use clinician-observed functional performance testing which matches patient self-report specific functional scores.
Do I need to use therapeutic exercise interventions before functional activity training, or can I skip a step and begin earlier with functional activity training?
Schedule visits/sessions at a location more conducive to observing and practicing functional movements, such as an athletic field, workstation, or patient’s home.
Collaborate with or refer to coaches, ergonomic specialists, or experts in the specific functional activities the patient expresses concern about in the patient self-report specific functional score.
The information on this website is not intended or implied to be a substitute for professional medical advice, diagnosis, or treatment. You are encouraged to perform additional research regarding any information contained available through this website with other sources and consult with your physician.
Damien Howell Physical Therapy – 804-647-9499 – Fax: 866-879-8591 At-Home, At Office, At Fitness Facility – I come to you, I do home visits Damien@damienhowellpt.com