Musculoskeletal pain which are important steps which are less important?
Thesis:
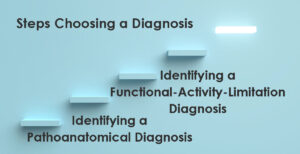
Choosing a diagnosis is an early step in solving non-traumatic muscle and bone pain problems. A diagnosis helps guide treatment, predict how problems will progress, and improve communication.
A diagnosis has many functions, including direction for intervention to solve problems, predicting how problems will progress, and assisting in communication.
Antithesis:
Medical terminology is notoriously complicated and often confusing. It uses Latin and Greek origins. The idiom “it’s all Greek to me” is germane. The eponymous custom of naming a diagnosis after a particular person can be problematic, such as Alzheimer's disease, Osgood-Schlatter disease, or Lisfranc fracture.
The lack of a clear explanation can be frustrating for both patients and clinicians, making diagnosis even more complex.
At its essence, diagnostic labeling is naming the problem. Naming the problem starts the process of answering questions.
Why did it happen?
What is the source of the pain?
What is the most appropriate intervention?
Which component of the problem should be a priority?
Not having an explanation is frustrating.
A common process of naming musculoskeletal-pain problems is to seek a pathoanatomical diagnosis. A pathoanatomical diagnosis identifies a specific tissue pathology presumptive to be the source or cause of an individual’s pain or dysfunction.
Diagnostic imaging identifying a pathoanatomical deviation has shown a weak correlation between structural findings and pain, failing to adequately explain why pain occurs.
Studies using diagnostic imaging of pain-free individuals can show pathoanatomical deviations such as:
- 90% with bulging neck disc.
- 66% of the shoulder rotator cuff tears.
- 69% hip labral tear.
- 68% knee cartilage damage.
Pathoanatomical deviations can occur without pain.
For me, as a Physical Therapist and/or as a patient when dealing with non-traumatic musculoskeletal pain, knowing a pathoanatomical diagnosis is a nice step, but is insufficient. Distinctly different pathoanatomical diagnoses can have remarkably similar interventions. Often, I do not have good interventions or logical mechanisms to specifically resolve the pathoanatomical diagnosis. Pathoanatomical diagnosis from diagnostic imaging studies may lead to unhelpful intervention.
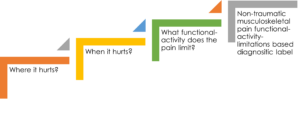
For non-traumatic musculoskeletal problems, an alternative to pathoanatomical diagnosis is a functional-activity-limitation-based diagnosis
The process of naming or diagnosing non-traumatic musculoskeletal-pain with functional-activity-limitations is identifying where it hurts. Then, when it hurts or what functional-activity is associated with the pain.
The following are hypothetical examples of diagnostic labels of non-traumatic musculoskeletal-pain with functional-activity limitations & accompanying pathoanatomical diagnosis.
| Where it hurts | Functional-Activity Limitation | Working hypothesis for intervention | Associated Pathoanatomical Diagnosis |
| Neck | When sitting for more than 30 minutes at work | If the arm rests on a chair can be adjusted to support the arms, then tension on the neck will decrease, increasing the amount of time sitting without neck pain | Cervical degenerative disc disease |
| Hip | After standing for more than 15 minutes | If a brief isometric strengthening exercise of the gluteal muscles is performed, then the ability to stand longer than 15 minutes without pain will occur | Acetabular labral insufficiency or tear |
| Knee Pain | When driving an auto for more than 30 minutes. | If the position of the foot on the gas pedal is altered from 3 o’clock to 1 o’clock, then pain will decrease. | IT band syndrome |
| Heel pain | When getting out of bed in the morning | If isometric exercises of foot intrinsic muscles (rock, paper, scissors) are performed before getting out of bed, then 1st step pain will be alleviated. | Plantar fasciitis |
| Thumb & index finger pain | After extended periods of crocheting | If a figure 8 splint is used on the thumb & index finger middle joint, then the frequency & duration of thumb and index finger will decrease. | Carpal tunnel syndrome &/or tenosynovitis |
Pathoanatomical diagnosis focuses on what is wrong (tissue pathology). In comparison, functional-activity-limitation diagnosis focuses on how it affects movement and function.
The idiom “what forest, I only see trees” is applicable.
A pathoanatomical diagnosis is like focusing on a single diseased tree in the forest, identifying its broken branches, decayed trunk, or diseased roots. It aims to pinpoint a specific structural issue causing the problem.
A diagnosis of non-traumatic musculoskeletal-pain with functional-activity limitation is like assessing the entire forest’s ecosystem, considering factors like soil health, climate conditions, and how the trees interact. This approach looks at broader functional patterns, movement impairments, and biopsychosocial influences rather than isolating a single structural defect.
Opting for a diagnosis of non-traumatic musculoskeletal-pain with functional-activity limitations instead of a pathoanatomical diagnosis has benefits that:
- Can lead to better patient outcomes.
- Reduce risk of reinjury
- Increase active patient participation in self-care.
- Increase in patient satisfaction and facilitate agreement regarding expectations between patient and clinician.
- Can be used immediately to initiate intervention or treatment regardless of whether a formal diagnosis has been made by a relevant health professional.
Synthesis
Of course, a thorough approach is to identify both pathoanatomical diagnosis and a diagnosis of non-traumatic musculoskeletal-pain with functional-activity limitation.
Reality is time, and resources are typically limited so choices must be made. Choosing to:
- Take every step in the process.
- Spend more time on a particular step.
- Spend less time on a particular step.
- Skip a step.
The step of choosing a pathoanatomical diagnosis is a step that requires less time and resources. The steps of identifying painful functional-activity-limitations deserve more time and resources.
Decisions about what steps we need to take, and which steps are nice to take, are determined by what gets measured. “What gets measured gets done” means that by tracking progress and performance, we are more likely to achieve a successful outcome. Measurement provides focus, motivation, and insights for priorities.

There are two mechanisms involved in the diagnosis and treatment of non-traumatic musculoskeletal-pain with functional-activity-limitations. One is pain and the second is functional-activity-limitations.
For non-traumatic musculoskeletal pain problems, identifying a specific functional-activity-limitation that is painful is a step that should not be skipped. Here is an example of this process is a Standardized individualized movement-evoked pain measurement.
Naming the functional-activity-limitation provides direction to the client and clinician on how to intervene. Here is a description of that intervention process. Intervention addressing functional-activity-limitations is a step that should not be skipped.

By prioritizing a functional-activity-based diagnosis alongside traditional pathoanatomical approaches, individuals and clinicians can create more effective, personalized treatment plans that lead to better outcomes.
The information on this website is not intended or implied to be a substitute for professional medical advice, diagnosis, or treatment. You are encouraged to perform additional research regarding any information contained available through this website with other sources and consult with your physician.
Damien Howell Physical Therapy – 804-647-9499 – Fax: 866-879-8591 At-Home, At Office, At Fitness Facility – I come to you, I do home visits Damien@damienhowellpt.com